Uterine fibroids (uterine leiomyoma) are benign, monoclonal, hormone-sensitive, smooth muscle tumours of the uterus2, 8. They are the most common benign tumours of the female reproductive tract in pre-menopausal women.
While literature-reported incidence rates for uterine fibroids vary, in part due to the large proportion of women who go undiagnosed, uterine fibroids are estimated to affect between 20% and 40% of women of reproductive age2. Uterine fibroids are reported to be more frequent in the mature age group (40% to 70% of women between 35 years and 50 years) 9,10.
Although a number of risk factors have been linked to the development of uterine fibroids, the causes of uterine fibroids are not fully understood11. Factors such as African or Black-American ethnicity, older age, family history of uterine fibroids, nulliparity (the condition of never having given birth) or lower parity (number of times a woman has given birth), and obesity have all been associated with a higher risk of developing uterine fibroids 11, 12.
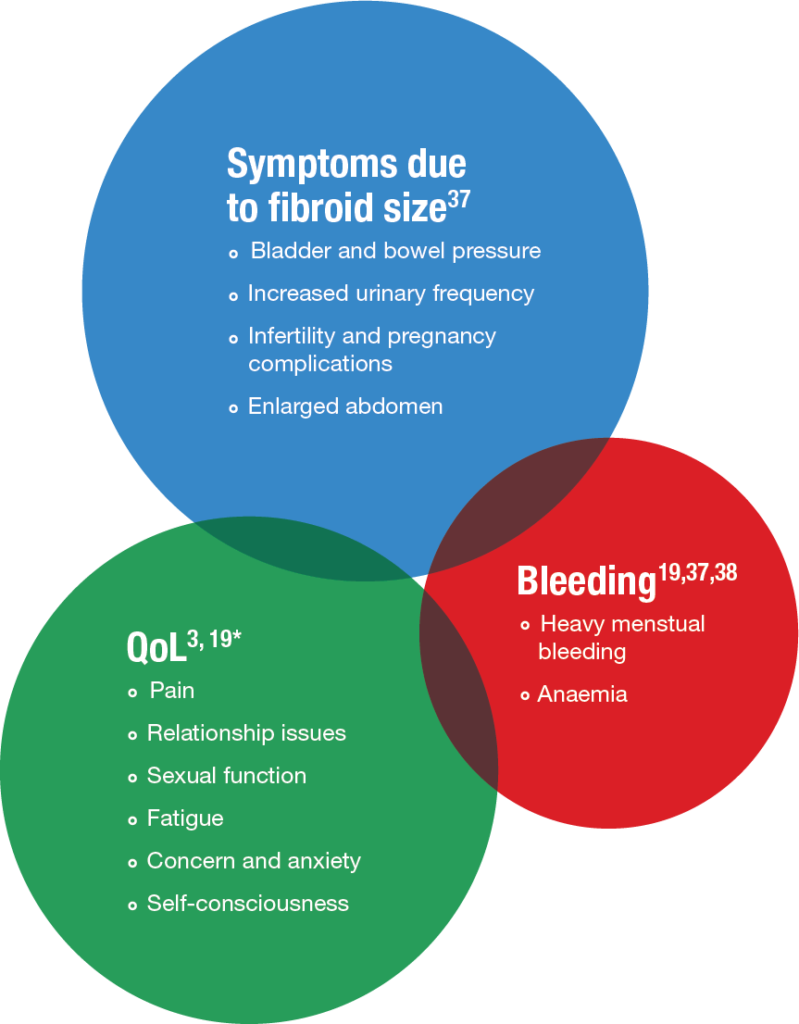
Uterine fibroids are often asymptomatic, but when symptomatic, the primary symptoms are heavy (uterine) bleeding, anaemia, abdominal pressure, abdominal pain, increased urinary frequency and infertility2. In particular, heavy menstrual blood loss is one of the most frequently disabling symptoms of uterine fibroids8.